Archive for May, 2018
Some Issues with Mid-level Medical Practitioners
Posted by Dr. Eric E. Shore, Esq. in Uncategorized on May 21, 2018
We have repeatedly seen posts online for and against so-called “Mid-level” medical practitioners and, truth be told, as a physician I have been known to pick sides in this issue. As a physician who is also an attorney, however, I believe the time has come for a legal perspective. First, though, I think it’s important to understand who these medical practitioners are, and why we began to produce them.
Decades ago, we could all see a shortage of what has been termed “Primary Care” physicians looming ahead. These generally include Internists, Family Physicians, and some Pediatricians; areas that fewer medical students were choosing because of the substantially lower reimbursement they received for their time than procedure-oriented specialties. The idea was a simple one. Some patients do not always require the level of knowledge and skill we learned in Medical School and Residency. A patient returning for a blood pressure check and some adjustment to their medication could probably be seen by (for example) a Nurse Practitioner. He or she might see the patient, note a slight increase in blood pressure and slightly increase the dose of medication while making another appointment for a recheck. Since all these advanced practitioners (“PAs”, “NPs or APNs”) were subject to oversight by a licensed physician who was in the same office, and who could answer any questions the NP had even before the patient left the office, or any error or oversight would be caught when they reviewed the patients’ charts, it was felt to be a safe and cost-effective way to supplement physicians’ ability so see more patients and so make health care more available and affordable. Moreover, originally these advanced practitioners were chosen from nurses who had many years of experience caring for patients, so while their formal education may have been abbreviated, their experience would go a long way toward their understanding of what they could handle, and what had to be referred to their supervisory physicians.
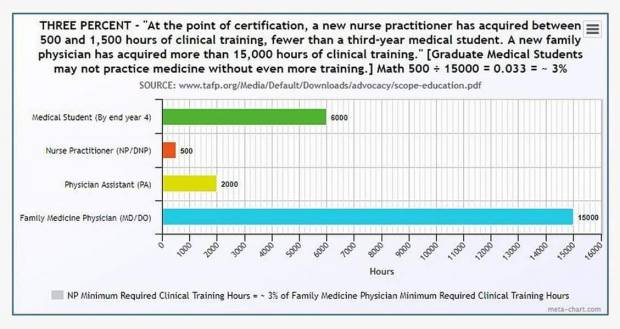
Since then, however, the original concept has been mangled to the point where many states have now allowed APNs to practice independently of physicians. This position has been advocated for by the insurance companies, of course, so they could pay out less money and some medical facilities for the same reason. This was followed by what have become diploma mills, many of which award Master of Science in Nursing (“MSN”) degrees and even a doctorate in Nursing Practice (“DNP”) purely online or with minimal hours “shadowing” a physician. The time and education it takes to become an APN or PA has been compared by some in the following charts:
The other issue is the definition of who is a “doctor” or, more importantly, how a patient can know who is really treating them since there are so many doctorates being awarded by so many different schools.
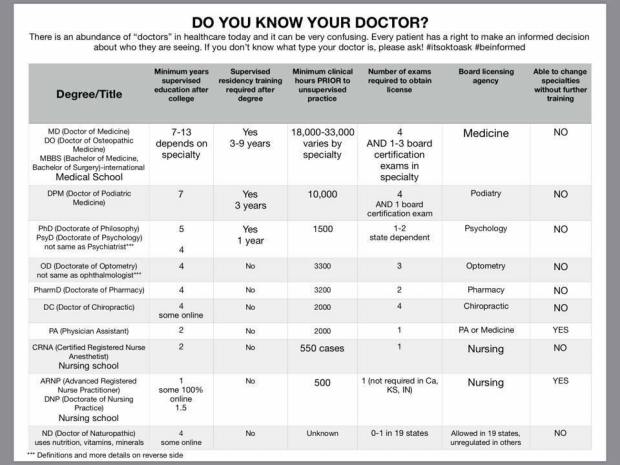
While I did not research these charts myself, I believe them to be reasonably accurate. Moreover, even if there are inaccuracies or inconsistencies, the reality is clear; the training MDs and DOs receive is many times greater that that of the mid-level practitioners.
The question now is whether the public is being best served under the “independent practice” statues that are being passed in some jurisdictions and, if not, how is a patient to know who is taking care of them? My answer to the first question is a resounding “NO,” and to the second, the only way to know in some cases is to ask. This should not be the case and what follows are some legal issues that physicians, and others, should pursue, with litigation if needed, to turn the tide.
The first, and most obvious issue is that of misrepresentation or, in some cases actual fraud. If an APN appears in a white coat whose name tag reads “Dr. J. Jones,” it is reasonable for a patient to assume they are a physician. In fact, some are now calling themselves physicians and there is even a new group who label themselves as “Cathopathic Physicians.” Moreover, while their license is for Nursing, what they do is practice Medicine with no oversight. Under these circumstances, these practitioners are clearly misrepresenting themselves and should be held liable under the appropriate circumstances.
The next issue is one involving malpractice. When a physician is negligent, they are held to the legal standard of a reasonable physician practicing in their specialty. Now, however, when an MLP is independently doing what physicians traditionally do when they practice Medicine, they should clearly be held to the standard of a physician doing the same thing. It is not reasonable to say they can treat patients, some of whom may not even realize they are not being treated by a physician or told that being treated by an APN is the same as being treated by a physician and hold them to a lower standard because their training is so much less. Imagine if an MD or DO who only had a few hours of training in the field performed neurosurgery, injured a patient, but was not held liable because they acted within the scope of their “training.” “Ridiculous,” you would say, but the analogy holds for NPs who practice independently. That must change and can only be changed through legislation (not likely today) or though litigation.
There are many other issues that need resolution, inter alia, from standardization of education to licensing standards and certification, and these can be covered in subsequent blogs, but the two mentioned above are both ones that, as a physician/attorney I would personally want to litigate. After all, I may be a physician, but I’m a patient also and I want the best care I can get when I become ill, and the ability to know the background of the person treating me.